The Eye
- FibonacciMD

- Mar 20, 2023
- 4 min read
Updated: Nov 15, 2024
A look at four common eye maladies: Arcus Senilis, Ectropion, Pterygium, and Pinguecula
Ophthalmology

InShort
by Evan Mostafa, MD and George J.Florakis, MD
Arcus Senilis
Arcus senilis, also referred to as corneal arcus, is defined by lipid and triglyceride deposits in the periphery of the cornea that lead to peripheral corneal opacity. The etiology is not well known, but it has been correlated with hyperlipidemia in the elderly and dyslipidemia in the young.
Signs and Symptoms
Arcus senilis causes a whiteish ring in the periphery of the cornea. Patients are typically asymptomatic.
Causes and Risk Factors
Risk of arcus senilis increases with age and is more prevalent among African-American males. The condition is also associated with cardiovascular disease (e.g., systolic hypertension).
Diagnostic Evaluation and Differential Diagnosis
Diagnosis of arcus senilis can be made during slit-lamp examination. A white circumferential band composed of triglyceride, cholesterol, and low-density lipid deposits appears in the periphery of the cornea. Laboratory tests may reveal elevated lipid levels. Differential diagnosis includes Terrien marginal degeneration and recurrent inflammatory limbal disease.
Treatment and Recommended Follow-Up
Because arcus senilis is asymptomatic, treatment is not usually indicated. Surgical intervention is also unnecessary. Visual prognosis is good. However, issues with lipid metabolism should be addressed.
Pearl to Know
Arcus senilis is common in patients with a familial history of familial hypercholesterolemia. Arcus deposition in one eye may suggest carotid artery disease on the contralateral side.
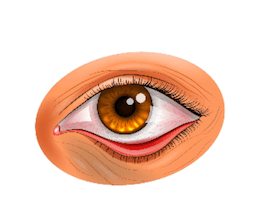
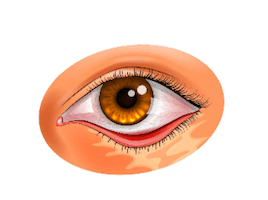
Ectropion

Ectropion is the eversion of the eyelid, which may lead to its separation from the globe.
Causes and Risk Factors
Causes of ectropion may be Involutional (horizontal tarsal laxity, medial canthal tendon laxity), paralytic (related to denervation of the lid protractors or paralysis of the orbicularis muscle (cranial-nerve VII palsy), cicatricial (shortening of the eyelid skin or both the eyelid skin and the muscle), congenital (congenital eyelid syndrome), or mechanical (tissue loss due to trauma, surgery, or thermal and chemical burns).
Eversion of Eye Lids
Diagnostic Evaluation and Differential Diagnosis
To evaluate the ectropion, routine ocular history and examination should take place, noting any previous eyelid trauma, surgery, nerve palsy, or contact dermatitis. In the snap-back test, the lid should return to its normal position with one blink after it is pulled from the globe. Abnormal laxity is present when it takes two or more blinks to reestablish the lid's normal position.
Treatment and Recommended Follow-Up
Treatment of ectropion includes corneal lubrication and lateral eyelid taping. In cicatricial cases, release of the cicatrix or a full-thickness skin graft may be indicated. Although mild congenital cases may not need treatment, other cases may demand treatment similar to that used for cicatricial ectropion.
Pearl to Know
When in doubt about the eyelid margin, look at the position of the meibomian-gland orifices, which are normally upright.
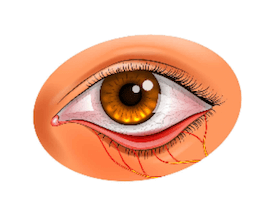
Pterygium

Pterygium is a common condition in which there is conjunctival degeneration that invades the superficial cornea. Pterygium is a noncancerous lesion consisting of conjunctiva and fibrovascular tissue that grows and invades the cornea which can interfere with vision. Pterygia can be bilateral or appear only on one eye. They may be nasal or temporal in each eye.
Signs and Symptoms
Burning and itching
Blurred vision
Foreign body sensation
If the pterygium grows significantly towards the visual axis, it can distort the shape of the cornea and cause astigmatism.
Causes and Risk Factors
Long term ultraviolet radiation from the sun
Dryness
Inflammation
Environmental risk factors such as warm climate, dust, and other irritants
A Pingueculum usually precedes the development of pterygium
Diagnostic Evaluation and Differential Diagnosis
An eye exam is often enough to diagnose the disorder.
Treatment and Recommended Follow-Up
Ultraviolet protection
Lubrication
Steroid eye drops for localized inflammation and swelling (usually not a chronic therapy)
Artificial tears may help reduce the symptoms that relate to dry eyes
Excision when the visual axis is threatened, there is significant astigmatism or if the pterygium causes considerable irritation.
Conjunctival autografts or the use of amniotic membrane and/or mitomycin C ,may decrease the recurrence rate.
Pearl to Know
100% UV block sunglasses can prevent or slow the growth of a pterygium, especially on sunny days, or near reflective bodies of water (ocean, lakes etc) or even from sun reflections days after a snowstorm.

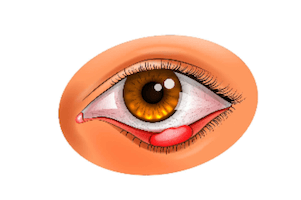
Pingueculum
Pingueculum is a common condition in which there is a non-cancerous growth (or degeneration) of the conjunctiva, usually in the part that is exposed when the eye is open (intrapalpebral). It is typically characterized by a yellowish and slightly raised thickening of the conjunctiva on the sclera, near the limbus of the cornea.
Causes and Risk Factors
Long term ultraviolet radiation from the sun
Dryness
Inflammation
Environmental risk factors such as warm climate, dust, and other irritants
Treatment
Ultraviolet protection
Lubrication
Steroid eye drops for localized inflammation and swelling (usually not a chronic therapy)
Artificial tears may help reduce the symptoms that relate to dry eyes
Surgical excision is rarely needed and is reserved if malignancy is ever a concern, or if patient has chronic symptomatic irritation (eg makes contact lens wear unbearable).
Pearl to Know
100% UV block sunglasses can prevent or slow the growth of pterygium, especially on sunny days, or near reflective bodies of water (ocean, lakes etc) or even from sun reflections days after a snowstorm.
Other Ophthalmology articles in this blog:
“Amblyopia - AKA Lazy Eye” by Emily Groenendaal, MD, and George J Florakis, M.D.
"Sudden Vision Loss: An Approach to Acute Vision Loss" by Eleni Florakis and George J. Florakis, MD
Sources:
Hashemi H, Khabazkhoob M, Emamian MH, Shariati M, Fotouhi A. A population-based study of corneal arcus and its risk factors in Iran. Ophthalmic Epidemiol. 2014;21:339–344.
Ang M, Wong W, Park J, et al. Corneal arcus is a sign of cardiovascular disease, even in low-risk persons. Am J Ophthalmol. 2011;152:864–871.e1.
Raj KM, Reddy PAS, Kumar VC. Significance of corneal arcus. J Pharm Bioallied Sci. 2015;7:S14–S15.
Macchiaiolo M. Buonomo PS, Valente P, et al. Corneal arcus as first sign of familial hypercholesterolemia. J Pediatr. 2014;164:670.
Vrabec MP, Florakis JG, eds. Ophthalmic Essentials. Cambridge, MA: Blackwell Scientific Publications, Inc; 1992:307-308.







Kommentare